Knee Arthritis
Total / Unicompartmental Knee Replacement
What is Knee arthritis?
 Arthritis leads to the weight bearing surfaces of the knee joint to become worn away. The cartilage layer is damaged and lost and is no longer smooth, this leads to stiffness and pain in the joint. Eventually the joint wears out to such an extent that the bone of the femur grinds on the bone of the tibia as most of the cartilage is lost.
Arthritis leads to the weight bearing surfaces of the knee joint to become worn away. The cartilage layer is damaged and lost and is no longer smooth, this leads to stiffness and pain in the joint. Eventually the joint wears out to such an extent that the bone of the femur grinds on the bone of the tibia as most of the cartilage is lost.
 The two common types of arthritis are osteoarthritis (generalised wear and tear of the joint which often is age related or post traumatic) and rheumatoid arthritis (inflammatory arthritis). The main indication for a knee replacement is worsening pain that has not resolved with non-operative measures (pain relief medications, weight loss, physiotherapy etc.) and is markedly affecting your quality of life.
The two common types of arthritis are osteoarthritis (generalised wear and tear of the joint which often is age related or post traumatic) and rheumatoid arthritis (inflammatory arthritis). The main indication for a knee replacement is worsening pain that has not resolved with non-operative measures (pain relief medications, weight loss, physiotherapy etc.) and is markedly affecting your quality of life.
Osteoarthritis either develops in just one compartment of the knee, inner (medial) compartment, outer (lateral) compartment or under the knee cap (Patello-femoral compartment), but can involve 2 or all 3 compartments of the knee as well. When only one compartment is involved, a uni-compartmental knee replacement (UKR) is the operation of choice and is designed to replace the worn joint surfaces on one side of the joint, thereby relieving pain and improving function. The operation can be performed through a smaller incision (around12cm – 15cm) which allows quicker healing and recovery.
If the arthritis involves more of the knee then a total knee replacement (TKR) may be recommended. This decision may sometimes be made at the time of surgery when the surgeon can directly inspect the joint surfaces. A TKR replaces the surfaces of the knee with metal and plastic in between. Sometimes a single fully plastic tibial component is used. Rarely the patellar surface (under the knee cap) is replaced with a plastic button, which glides over the metal surface of the femoral replacement, however when the patella is satisfactory, it may not require surgery. To be able to replace the surface of the knee joint a 20cm incision is made down the front of the knee and the joint opened. The arthritic joint surfaces are removed and the bone is shaped so that the joint replacement components can sit firmly on the bone. The replacement parts are positioned and held in place with bone cement.
Benefits of a Total / Uni-compartmental Knee replacement
The main benefit of this type of surgery is relief of pain. Patients may also notice an improvement of function, allowing them to walk easier and further. Daily activities should become more comfortable and quality of life improved. Some patients may find an improved range of movement after the surgery, although this cannot be guaranteed. The main predictor for range of motion after the operation is range of motion in the knee before the operation.
Before Surgery
Exercises to do
Being active while you wait for surgery is important. People with a painful knee joint are often afraid to be physically active because they worry they may be doing more harm than good. This is not the case. In fact, research has shown that exercise can help decrease pain, improve leg strength and help keep your heart in good condition before surgery. If you have not been regularly active, remember to speak to your GP before starting to exercise.
Endurance activities are good for your heart, lungs, circulation and muscles. Some suggestions for endurance exercises include walking, swimming or use of a stationary bike. If you have not been involved in any regular exercise, it is important to start slowly. Your goal is to be physically active every day. Begin with a few minutes and gradually progress until you can exercise at least 3 times per week for 20 to 30 minutes at a time. No matter which activity you choose to perform, you should be able to carry on a conversation or talk comfortably while exercising without an increased shortness of breath.
Being involved in an exercise program before your surgery will help in your recovery after surgery. After your surgery a team of physiotherapists, occupational therapists and nurses will help you regain your strength, endurance and improve your overall function.
Walking and leg strengthening exercises are an important part of your rehabilitation after your joint replacement surgery.
Guidelines for Performing your Strengthening Exercises
Repetitions
Each exercise should be repeated several times until you feel some tiredness in your muscle. As you get stronger, you can add more repetitions or sets, continuing to use muscle tiredness as your guideline. If an exercise continues to cause you excessive pain that doesn't go away, stop doing that exercise.
Frequency
1 – 2 times per day
Duration
Hold desired position for 5 seconds before releasing.
Exercises for Patients Scheduled to Have Knee Replacement
Please note: In the instructions, involved heel/leg indicates the leg, which will be undergoing surgery.

Knee Leg Press (Beginner exercise)
- Sheet around heel of involved leg
- Bend knee using the sheet
- Straighten your leg against resistance of the sheet
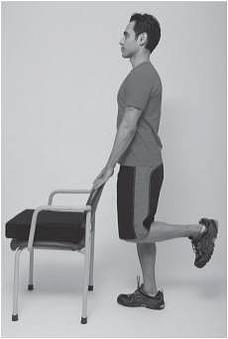
Standing Hamstring (with or without weights)
- Hold on to a chair or place your hands on a wall
- Bend knee so involved heel moves towards buttock on the same side

Isometric Hamstring
- Bend involved knee against resistance from opposite foot
- Just tighten muscles, do not move legs

Chair Push-Ups
- Sit with hands on arms of chair
- Push down on hands to lift buttocks off chair

Toe Raises
- Rise up on your toes by lifting your heels as high as possible
- You may want to use the back of a chair or countertop for balance
Prepare your home
There are a number of things you can do before your surgery to help get prepared:
- Tell your family and friends that you are having surgery and might need their help during your hospital stay and after your discharge home.
- Ask someone to help you with household tasks such as grocery shopping, house cleaning and laundry.
- Arrange transportation to and from the hospital on day of surgery, discharge day and first follow-up visit.
- You cannot drive for the first 6 weeks after surgery, so make other arrangements to get to appointments, etc. If you rely on community services for transportation, make sure you arrange for this in advance.
- If possible, cook and freeze meals ahead of time.
- Be sure your shower or tub has a non-slip coating or mat.
- Obtain necessary equipment to help you manage your activities safely (see next page for details).
Select a coach
This optional program gives you an opportunity to choose a family member or a friend as a "coach" who will help you before, during, and after your hospital stay.
Your Coach should:
- Attend the consultation/ joint school and Pre-operative assessment visit with you
- Help you plan for your admission to hospital
- Help you prepare for your discharge home
- Translate if english is not your first language
- Be a "second set of ears" to help remember instructions
- Come with you to the hospital on the day of surgery
- Be available when you are discharged home to help you settle in, and remind you of all your instructions
Nutrition and Weight Management
Eating a well-balanced diet, as recommended will help your body heal. Extra weight can also affect your recovery by reducing your exercise tolerance. Talk to your doctor/ dietician about an appropriate weight loss program if needed.
Dentist
Remember, your dentist is an important part of your healthcare team. Bacteria from an infection in your mouth can travel through your bloodstream to your new joint causing infection there. So make sure any tooth or gum problems are treated before your surgery. Also note, following your surgery, you will need to let your dentist know that you have had a joint replacement as you will need antibiotics before any dental treatment.
Illness before surgery
If you develop cold, flu, or gastric symptoms (such as diarrhea) before your surgery, please call the admissions office or my secretary. If surgery must be postponed because of illness, we will make every effort to arrange a new surgical date as a priority.
Protect yourself from falls
Arthritis of the knee can increase your risk of falls. There are a number of things you can do to decrease this risk before and after your joint replacement surgery.
Consider these practical suggestions:
- In the kitchen, do not use a footstool to reach for objects.
- Move frequently used items to lower shelves.
- In the bathroom, equipment such as raised toilet seat, grab bars or a tub seat may be helpful. An occupational therapist can help determine which aids would be most helpful for you. Everyone should use a non-slip rubber mat or self-stick strips on the floor of the tub or shower.
- Put a nightlight on the path from the bed to the bathroom if the area is normally very dark.
- In the bedroom, make sure there is a bedside lamp in easy reach so that you can turn it on if you have to get up during the night.
- Always get up slowly after sitting or lying down.
- Take your time when going up or down the stairs. Be sure that stairways are well lit, free of clutter, and have a secure handrail.
- Stairway carpeting should be secure.
- Remove throw rugs.
- Pathways should be cleared of cords or wires by coiling or taping them to the wall.
- If you have pets, consider removing your pet from the home during your early recovery stage or arrange for family/friends to take your dog out for walks. Be careful of active or sleeping pets as you walk. Place a bell on their collar so you are aware of their movements. Try to keep pet toys in a designated area to reduce the risk of tripping over them.
- Never rush to answer the telephone. Ask friends/family to allow the phone to ring many times, allowing you time to answer. An answering machine or a cordless phone can be helpful.
- Keep emergency numbers in large print near each phone.
- In the garden, put tools away, wear supportive shoes and avoid walking on wet grass.Use your walking aid indoors and outdoors if one has been prescribed.
- Be sure indoor and outdoor shoes fit properly. Footwear should have support around the heel and rubber soles. Try elastic or Velcro shoes if you have difficulty tying laces.
- Do not carry too many packages (use home delivery or pushcart).
- When walking outdoors, avoid walking on poorly maintained sidewalks, unlit streets and icy surfaces.
- Try to walk with a walking partner. Consider other options such as walking in a mall for exercise.
Pre-operative assessment clinic
You will receive a letter to attend a pre-operative assessment clinic (POAC) a few weeks or so before your planned surgery. Your visit to the POAC is to help you prepare for your operation, discharge home and recovery. The POAC is run by a team of specialist nurses. At the POAC your medical fitness for an anaesthetic will be assessed and any tests required organised. Most people require some blood tests, urine tests and a heart tracing (ECG). Occasionally other tests are required depending on your state of health. You may meet a physiotherapist who will show you some exercises for after the operation. An occupational therapist may discuss with you any adjustments to your home situation that may be helpful for your discharge.
